H5N1 in Retail Raw Milk in California Again - This Time Herd Bulk Tank Presumptive Positive at CDFA
So, if we don't diagnose H5N1 in raw milk drinkers, does that mean the scientists have lied to us again about risks?
Another week, another set of articles in the erstwhile New York Times warning of the impending pandemic threat from H5N1…
NYTimes-A Bird Flu Pandemic Would Be One of the Most Foreseeable Catastrophes in History
Opinion | I Ran Operation Warp Speed. I’m Concerned About Bird Flu. - The New York Times
While avian-derived strains are now stealing some of the thunder by infecting poultry flocks with devastating effects in Canada and in rapidly spreading areas of the U.S., B3.13 continues its assault on California dairy cows with the herd infection rate now approaching 50% of the state’s dairy population. Early infected herds are reportedly nearing a return to negative herd status, at least for now, while a twice retail-implicated raw milk herd was PCR positive on a second weekly test.
Dr. Kay Russo with RSM Consulting LLC has summarized 2-month commercial poultry depopulations well in LinkedIn. In another post she stated that roughly half of California’s layers have now been depopulated. Current poultry losses are dire enough; however, the efficacy of contemporary H5N1 B2.3.4.4b viral strain(s) in infecting “bio-secure” poultry operations seems unprecedented, given the rate of new infections across diverse geographical areas and poultry production types. Additional poultry industry losses across all of the U.S. for the remainder of this winter-early spring seem nearly inevitable. I can’t help but think that egg and poultry meat shortages and high prices will be a huge economic crisis by early spring for consumers.
Dairy production losses are less publicized, and H5N1 in dairy herds seems to be fairly quiet outside of California, at least from a clinical case standpoint. Upcoming planned regular bulk tank testing across most states will provide a clearer picture of actual national incidence and may also uncover “hotspots” of infection that have been ignored through lack of testing.
We also lack data on what reinfections may entail in recovered herds. Will pre-existing immunity from prior infections tamp down the severity of subsequent herd infections? Or will it drive viral diversity towards non-neutralized strains with full subsequent outbreaks in recovered herds? One of the real flaws in the current testing scheme is our lack of aggressive systemic monitoring of recovered herds for reinfection and genomic analysis of any viruses recovered. Routine bulk tank screening should resolve this issue if it is implemented with the new administration.
We are past the point where counting “total herds infected” and “all states affected” are valuable metrics for dairy H5N1. Areas of states with active infections (positive bulk tanks) and genotypes of viruses recovered are much more critical, along with metrics on human exposure maintained in collaboration with public health authorities.
Eradication of H5N1 is likely impossible in the short term in the dairy industry. The shorter-term goals should be to minimize replication through movement biosecurity and (hopefully) vaccination and then maximize transparency through repeated isolations and sequencing of new infections. Those isolations should not stigmatize a herd; rather timely reporting should be programmatically rewarded and required.
While the virus may not economically devastate dairy production, U.S. agriculture cannot expect that poultry, beef, and swine industries will remain viable if H5N1 just moves unmonitored and uncontrolled in prevailing endemically infected dairy cattle flows. Status quo non-reporting with relatively unrestricted movements of cattle with unknown H5N1 status is not sustainable in the dairy or beef industries. The situation will become even less sustainable if (or when) the virus begins to differentiate and/or reassort into multiple strains with varying degrees of animal and human pathogenicity and infectivity.
Raw Milk
The most concerning zoonotic-related news of the week came from California on Friday, when Mark McAfee, the CEO of Raw Farms, a relatively large raw milk supplier in that state, announced that the second week of California Department of Food and Agriculture (CDFA) testing of his herd found evidence of H5 virus in bulk milk samples, following a second positive retail sample uncovered by the California Department of Public Health (CDPH) in 2 weeks:
Distribution of Raw Farm's products suspended amid bird flu concerns
I won’t add to the comments from Mr. McAfee regarding his interpretations of his herd’s status over the past several weeks; suffice it to say that any dairy herd near Fresno in late October-November 2024 has been at dire risk of H5N1 infection due to location in the epidemic area alone.
The bigger point is that several thousand California consumers have directly consumed raw milk with significant levels of viable H5N1 B3.13 virus in the product. This has generated a giant retrospective non-standardized non-case-controlled H5N1 Select Agent variable oral dose infection experiment in human volunteers! This will be an interesting exercise from which many will attempt to draw conclusions related to a very controversial contemporary issue…H5N1-infected raw milk consumption!
Assessing the results of this known exposure is a public health undertaking well beyond my pay grade, worthy of national CDC-public health institution assistance to local and state officials who are already overtaxed in dealing with the H5N1 dairy and poultry outbreak public health fallout. Despite all the challenges, CDPH, local health departments, CDC, and academic partners must do as much as possible to monitor for ILI and nonspecific illness, including widespread genotyping of any positive influenza samples. Hopefully a cadre of volunteer raw milk consumers can be recruited for serial antigenic and serum sampling post exposure, the sooner the better! Time is of the essence because any illness or subclinical infection accruing from consumption of this product is likely to show up now or very soon, with PCR evidence fading as active infection fades. Obviously, area clinical records will be assessed for any deviations in morbidity/mortality from the norms. Due to seasonal flu now circulating, the risk of reassortment is also a possibility, so subtyping and sequencing of flu isolates in the area will be critical to assess that risk.
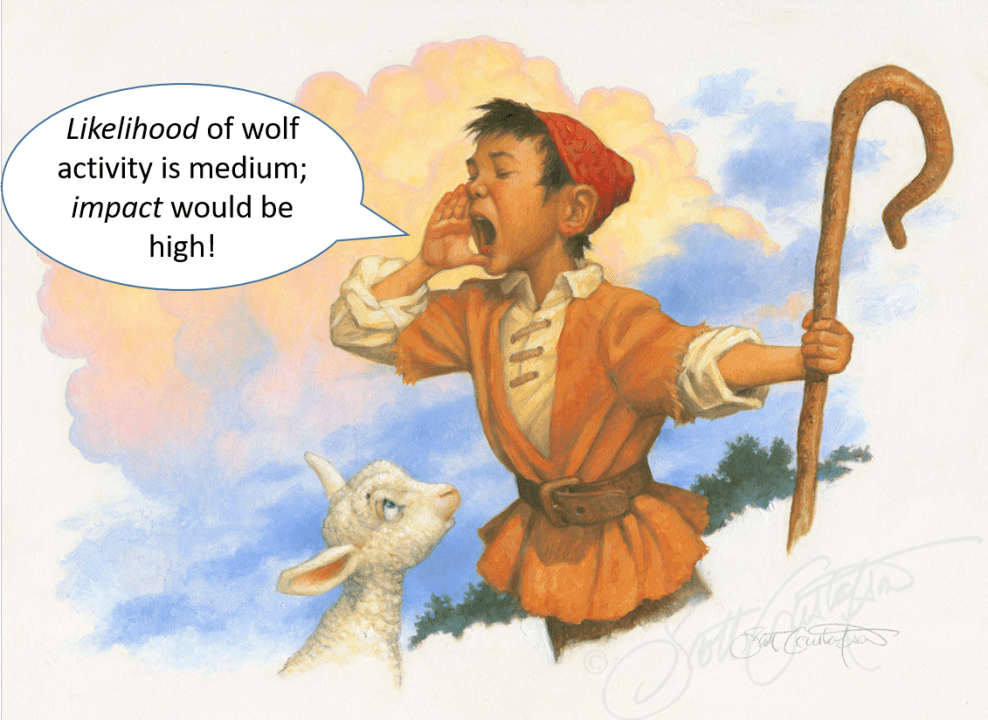
I think it is important to state up front that we may no or very little illness associated with oral consumption of H5N1 B3.13. It’s known to be lethal to mice and cats, and ARS showed it infects dairy calves orally; however, species susceptibility to influenza genotypes varies. The danger is that the public in general extrapolates an observation from one influenza virus to all of them, i.e. if the current B3.13 should prove to be fairly innocuous for humans in raw milk at doses found in this California “experiment”, that does not extend to ALL H5’s or even all H5N1 B3.13 viral reassortants with other influenza viruses.
Another caveat that may or may not play out in this California scenario; all peoples’ resistance to a given agent are not equivalent. Immunocompromised, the young, elderly, certain human genetic subtypes, etc. may have very different susceptibilities to a virus that has no effect on 95% of the population. Biological variability is a significant risk factor not to be minimized as numbers of exposures become high enough to overcome natural barriers like receptor site incompatibilities or inadequate dose presentations.
Finally, as I alluded to earlier, we face the constant threat, especially in pigs and people, of viral reassortment with endemic influenza. While H5N1 2.3.4.4b B3.13 may be subclinical in people, it could reassort with seasonal H1N1 or H3N2 to form a new reassorted virus with enhanced pathogenicity, infectiousness, and/or antiviral resistance. “H5N1 doesn’t make me sick” doesn’t mean that its reassorted offspring couldn’t make lots of people very sick…
So why can’t we reassess all this foolishness and just ban raw milk sales? I came across an article today from Popular Science that elegantly lays out all the “science” and takes on all the arguments made by raw milk proponents:
Is raw milk safe? Science has a clear answer. | Popular Science
The article makes a detailed and cogent case for NOT allowing the sale and consumption of raw milk to the public, as well as pushing back on some of the common benefits given for its consumption by advocates.
Partly in response, here is Mark McAfee of Raw Farms in a PBS News piece:
Raw milk sales spike despite CDC’s warnings of risk associated with bird flu | PBS News
Still, testimonies to raw milk are trending on social media sites. And Mark McAfee, owner of Raw Farm USA in Fresno, California, says he can’t keep his unpasteurized products in stock.
“People are seeking raw milk like crazy,” he said, noting that no bird flu has been detected in his herds or in California. “Anything that the FDA tells our customers to do, they do the opposite.”
Much like some of the commentary surrounding the election and related to the nomination of RFK as HHS Secretary, distrust of authority and science has become a feature, not a bug, in public opinion! Similar to antipathy towards the mRNA vaccines, a significant portion of the public fervently believes that “they” (the federal scientific community) are out to mislead them, and the best path is to resist whatever consumers are advised to follow.
I have a well-informed friend who firmly believes that raw milk has “saved his life” from a physiological perspective. We’ve even discussed the “placebo effect”, which I suspect may be at play with him; however, no amount of research or especially lecturing from me about complicated viral health risks “you really wouldn’t understand” will change his mind.
My point is that we are not going to repeal state-based raw milk exemptions in the short or intermediate term short of catastrophic mortality events. If we view H5N1 in raw milk as a threat (which I believe it truly is), we must work with product testing, biosecurity, and vaccines to lower risks for finding virus in the milk. We can also work on consumer education over the longer term, but it is not a short-term solution in the current political environment.
In fact, it’s possible that FDA and CDC will be directed by incoming HHS leadership to “stand down” in warning consumers of the dangers of raw milk consumption, according to some news reports of aspirations by the new administration’s leaders. It will be interesting to see how science-based agencies will craft these messages.
Righteous indignation, demeaning condemnations, and educational aloofness are the worst possible routes to affect change right now. It may be time to just listen, do our best to really observe and record real events, then hold genuine smaller conversations regarding a whole host of scientific endeavors. We’ve lost the “elite perch” that we had presumed to provide us our credibility. Honesty, transparency, and good will always win out, but we have to bring some of the currently disaffected public with us to once again be trusted as credible knowledge workers.
John