Hail the Revolution but Mind the Alligators!
The H5 situation in California and elsewhere continues to deteriorate at a dizzying pace, as new leadership is named at the federal level to "Make America Healthy Again"
Once again my articulate colleague Dr. Kay Russo with RSM posted a great summation of the past week’s new related to H5 in cattle, poultry, and people
Kay Russo - RSM Post 1- cows and birds | Feed | LinkedIn
Kay Russo-Post 2 -Human | Feed | LinkedIn
As usual CIDRAP also provided a great summary on Friday of recent news
CDC confirms H5N1 in California child as Hawaii details testing results | CIDRAP
For today, I’d like to stick to some “big picture” impressions I took away from a swine industry H5N1 webinar as well as from further developments as covered by Kay and CIDRAP in this past week’s review of the H5 whirlwind of events in Canada, U.S., in poultry, cows, and people.
Perhaps the most alarming summaries in the news this weekend came from articles I came across courtesy of links found on Sharon Sanders’ FluTrackers.com: The first is an interview with the President of the California Poultry Federation: California’s avian influenza outbreak escalating - Brownfield Ag News
The President of the California Poultry Federation is concerned about the speed highly pathogenic avian influenza is spreading in his state.
“If it doesn’t slow its pace in the next month, we’re in serious trouble.”
Bill Mattos tells Brownfield California has been able to avoid the disease for a long time, but interstate cattle movement has escalated the current outbreak.
“Unfortunately, most of the dairies and the poultry industry is right next to each other from Sacramento to Bakersfield, that’s where we grow everything,” he shares. “The quarantine areas are set up immediately if a dairy is checked positive and there are already 400 dairies positive.”
Mattos says producers are on high alert with enhanced biosecurity measures.
“The veterinarians are warning people that we have to look at every avenue to try to stop this disease because we don’t know if it’s sustainable if we keep going like this,” he shares. “The way we’ve seen it in California the last two, three weeks—it’s very scary.”
The California Department of Food and Agriculture reported its first case of the virus on a dairy farm at the beginning of September and cases have increased to 402 as of Wednesday.
In the last 30 days, the USDA says 22 commercial flocks have been affected and more than 5.2 million birds have been depopulated in California.
The state has also confirmed 29 human cases of the virus with nearly all of them linked to cattle exposure.
Let that sink in - 402 dairy herds, 22 commercial poultry flocks with 5.2 million birds, and 29 KNOWN human infections just in California through November 22nd, plus an “unattributed source” H5N1 human infection (genotype still not released by CDC). As Kay Russo so passionately states, we lack timely genotype information on the California poultry outbreaks; however, many are likely from dairy cattle genotype exposure.
I would actually go further than Mr. Mattos states above; I think poultry production in California is already doomed into the winter as the dairy outbreak plays out. We have shown no ability in any state with concentrated dairy populations to stop viral spread between dairy farms or to poultry operations. Further, we have not been able to control human exposure in workers on farms or in response activities. All of our guidance for increased biosecurity and worker PPE have met with minimal success in stemming the spread of this virus across the Central Valley in California. We witness virtually unchecked intra and inter-herd area spread within cattle herds and between cattle herds, poultry flocks, nearby people and other susceptible species. I hope our universities and researchers currently have staff on the ground documenting viral loads in communities and testing area spread theories as this plays out. The virus is undoubtedly also spreading into peridomestic species and domestic pets, all which should be closely monitored and tested.
Feral pigs and outdoor swine are obvious high-priority targets for enhanced surveillance, if state and federal resources can be mustered to partner with local resources in voluntary enhanced surveillance efforts. This would be a great place for national and state swine organizations to enhance efforts with local producers to proactively screen for potential early cases of H5 in highly exposed swine populations. If the swine industry is to avoid establishment of a reassorted H5 virus in the commercial swine population, it must find early incursions of the strain in pigs in high-risk areas before those infected pigs can mingle with endemically infected pigs in marketing chains, exhibitions, etc. Isolation and elimination are feasible in small batches of swine in remote areas. Once the virus reassorts, replicates, and spreads into the commercial marketing and exhibition sectors, vast segments of commercial production are at risk for infection, making elimination much more painful or impossible.
We really can’t have reassorted H5 swine viruses endemic in commercial swine production. The zoonotic risk scenario with ongoing endemic reassortment is completely different than for H5N1 2.3.4.4b B3.13 in dairy. Business as usual will not be tolerated with partially-human-adapted H5 viruses in respiratory circulation in swine herds! Any aspirations for “business continuity” planning in this scenario is a pipe dream.
I do want to congratulate my colleagues in the swine industry for developing and hosting a timely (in under 3 weeks) public facing webinar titled H5N1 Influenza Risk to US Swine held on Wednesday, November 20. USDA-APHIS confirmed the diagnosis of H5N1 in backyard pigs housed with a mix of poultry and other livestock on a small Oregon farm on October 30, 2024. This webinar was hosted by the Swine Health Information Center and the American Association of Swine Veterinarians and produced by the Swine Medicine Education Center at Iowa State University.
Here is a list of the speakers and topics covered:
Ryan Scholz, DVM, MPH, State Veterinarian, Oregon Department of Agriculture
Overview of the first detection of H5N1 in a pig on a backyard multispecies farm in OR
Montse Torremorell, DVM, PhD, Dept. Chair and Professor, University of Minnesota
H5N1 risks to swine and knowledge gaps for prevention and preparedness in pigs
Fred Gingrich, DVM, Exec. Director, American Association of Bovine Practitioners
H5N1 impact to the dairy industry and update on diagnostic surveillance
Bailey Arruda, DVM, PhD, Research Veterinary Medical Officer, USDA ARS
Update on H5N1 experimental infection studies in pigs
Locke Karriker, DVM, MS, Vet. Diag. and Production Medicine, Iowa State University
Update on aspirin use in pigs
I’ll cover the webinar in more detail after the recording is available for review to assure accuracy. Big take homes for me:
the infected pigs were intimately mixed with lethally infected poultry, making for high direct infectious doses for these “non-traditional” pigs. Regardless, the pigs were systemically infected- these were not simply “contaminated” PCR positive cases.
the ARS-NADC research is ongoing and now has placed 9 different H5N1 2.3.4.4b viruses (including 3 B3.13 isolates) in pigs. All 9 strains have been shown to infect pigs to differing degrees, with differing clinical signs and degrees of onward transmission. Generally, clinical signs and lesions are mild (respiratory, digestive, neurological) and not consistent, and onward spread is also somewhat sporadic.
potential for reassortment has not yet been investigated (gain of function hurdles), nor has the Oregon strain yet been directly tested in laboratory studies. Stay tuned…
The bottom line is that potential for spillover into pigs is still a hard-to quantify risk, given the above factors. However, pigs CAN be infected and can transmit the virus onward. Given that evidence, I think we must assume that possibility and aggressively continue to look for viral evidence in pigs in high-risk areas.
If the California situation is not dire enough, another FluTrackers link summarizes the situation in Canada, as reported by CFIA:
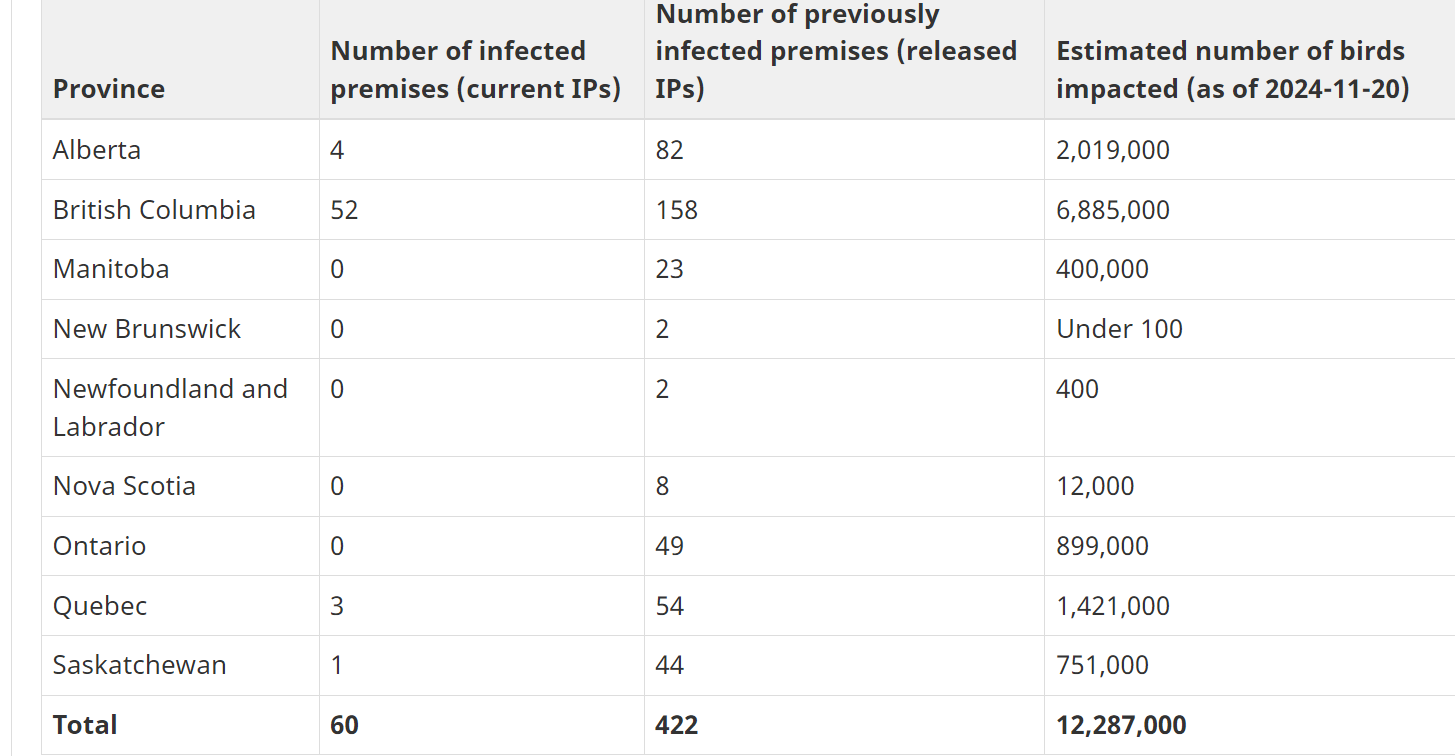
Status of ongoing avian influenza response by province - inspection.canada.ca
Canada currently has 60 premises under quarantine without dealing with the dairy strain, all due to wild bird contamination or spread from other infected premises. Canada has reported no human infections from occupational exposure but has reported an H5N1-infected critically ill juvenile in British Columbia. The source of the patient’s infection remains unclear.
It’s important for us to remember that domestically in the U.S., our fall-winter wild bird migration high risk period is just beginning, with recent new H5 detections in backyard flocks in Illinois, South Dakota, Colorado, Montana, Utah, and Pennsylvania. As the birds migrate, we are likely to see some of our commercial poultry operations outside of California also succumb to H5. Thankfully, H5N1 2.3.4.4b B3.13 has remained quiet outside of California (except Utah and perhaps Oregon with recent H5 poultry outbreaks in dairy areas). As bulk tank testing kicks in and cattle movements intensify, we may also see some resurgence of reported dairy H5 outside of California.
As of Saturday, President-elect Trump has nominated new cabinet-level appointments for USDA (Brooke Rollins), FDA (Dr. Martin Makary) and CDC (Former Congressman Dr. Dave Weldon). None of the “highlight articles” mention the upcoming challenges that these people will face in dealing with H5N1 in dairy cattle, poultry, and people. Confident campaign promises about “deconstructing the administrative state”, “lowering the cost of eggs and milk”, lowering federal mandates, and allowing vaccine choices are about to come face to face with a vicious virus causing billions of dollars in losses, crippling food production capacity, and greatly increasing risk for further H5 viral exposure to a wide swath of susceptible animals and people.
An article today in the Washington Post examined the new cabinet choices’ records related to fighting disease outbreaks:
Trump health picks largely untested in fighting disease outbreaks - The Washington Post
I truly wish these people and their deputies the best; if they want to avoid catastrophic losses, including lives, they must quickly learn some lessons from the scientific establishment many have been so quick to condemn in the heat of the election. The staid pharmaceutical-agricultural-research establishment does need to be challenged with fresh leadership; however, we must not throw out all our great advancements in the name of radical under-tested revolutions in our research and regulatory approach that some now advocate.
The principles of infectious disease control are not altered by elections. We in regulatory medicine have always dealt with tension between individual freedom versus group conformance in establishing protocols and prevention measures to maintain corporate animal and public health. A regression to much less federal oversight of animal and human health disease management is likely to aggravate spread of highly infectious diseases like H5N1 in the face of widespread interstate and international movement and trade that exists in today’s world.
H5 may or may not become a full-blown zoonotic pandemic; regardless, it is already a full-blown agricultural crisis for both the poultry and dairy industries and a grave potential threat to the swine industry due to ongoing reassortant/zoonosis risk. It is an ecological disaster for nature and the environment with ongoing and yet unforeseen consequences. I hope that our new leaders will join all of us in facing this crisis with open minds for control to complement a fresh set of marching orders for dealing with it.
Mind the alligators,
John